In the world of pregnancy, there’s a critical term you should be familiar with – Intrauterine Pregnancy (IUP). If you’re wondering what this means and why it’s so crucial, you’ve come to the right place. According to National Institutes of Health, The accuracy of IUP might be as high as 90%. In this comprehensive article, we’ll explore the ins and outs of IUP, from what it is to how it’s diagnosed, and what factors can affect it. So, let’s dive into the fascinating world of Intrauterine Pregnancy.
What is Intrauterine Pregnancy (IUP)?
An intrauterine pregnancy, commonly referred to as IUP, is a term used to describe a pregnancy where a fertilized egg successfully implants and develops within the uterus. It’s important to note that the uterus is the only place in the female reproductive system where a pregnancy can thrive and progress to full term. Any pregnancy that occurs outside the uterus, in areas such as the cervix, ovary, or fallopian tubes, is termed an ectopic pregnancy and is not viable, meaning it will not result in the birth of a child.

How Is an IUP Confirmed?
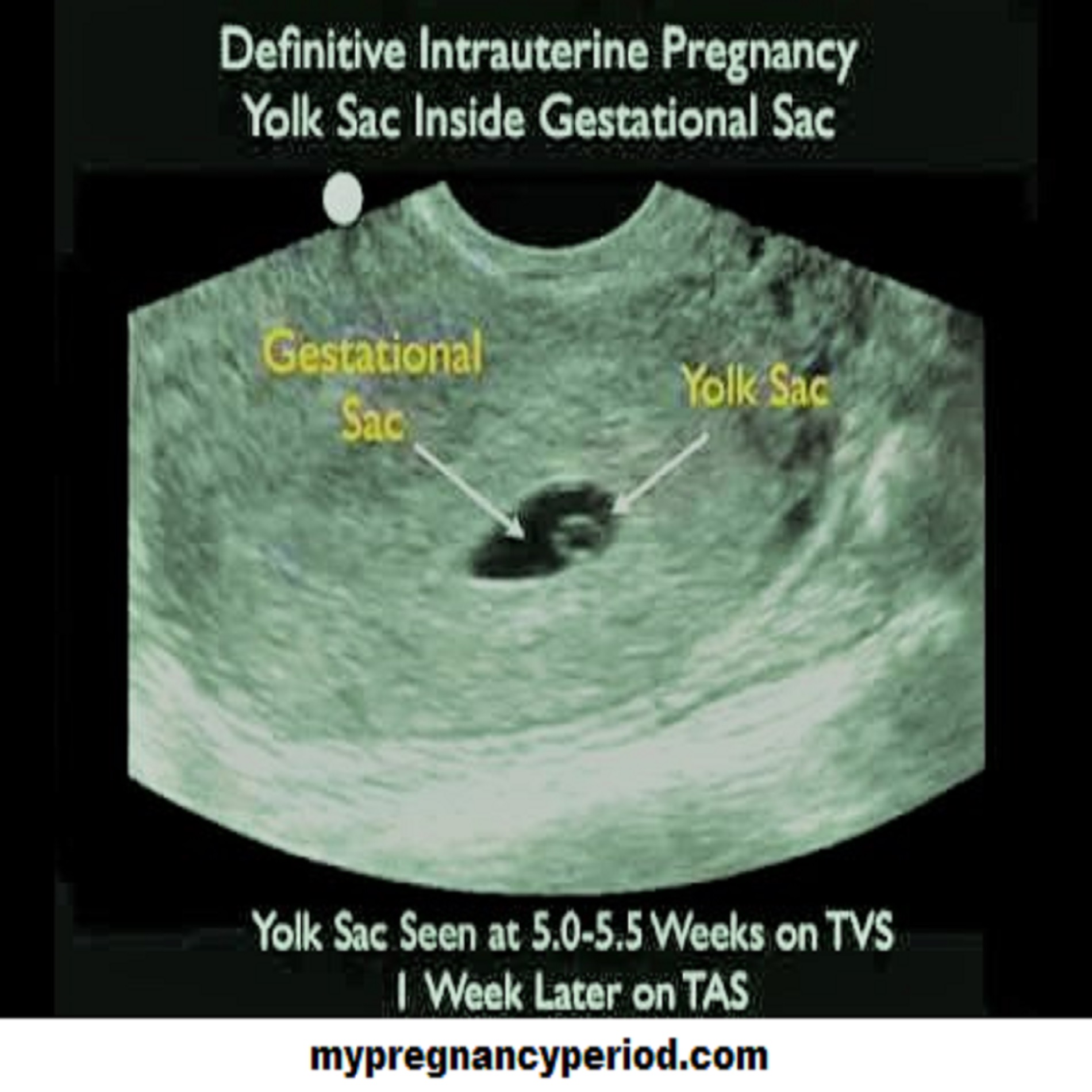
The confirmation of an IUP is typically done through an ultrasound scan. There are two key indicators that healthcare professionals look for during this scan:
a. A Visible Yolk Sac
Around 5.5 (or 6) weeks into gestation, a transvaginal ultrasound can reveal the presence of a yolk sac. This sac provides essential nutritional support for the developing embryo until the placenta fully forms. It is the primary element that confirms the presence of a live intrauterine pregnancy until an embryo is visible.
b. An Embryo with Fetal Heart Activity
Fetal heart activity can be detected as early as 6 weeks into gestation. The normal heart rate for a developing fetus ranges between 100-120 beats per minute (BPM) and gradually increases over the subsequent weeks. It’s worth noting that a heart rate below 80 BPM before 6.3 weeks is associated with a higher risk of miscarriage during the first trimester.
What Is an Early IUP?
An early intrauterine pregnancy occurs when a gestational sac forms in the womb during the early stages of pregnancy. It does happen for two core reasons:
a. Uncertain Conception Date
In some cases, the mother may not be sure of her exact conception date, has irregular menstruation, or recently stopped using birth control. This uncertainty can lead to the appearance of an early intrauterine pregnancy.
b. Irregular Growth Rate
Sometimes, a pregnancy’s growth rate may not align with the expected timeline. This can also result in the diagnosis of an early intrauterine pregnancy.
How to Spot an Early Intrauterine Pregnancy?
The typical method for diagnosing an early intrauterine pregnancy is through a positive result on a pregnancy test. Following a positive test, a transvaginal scan is performed to confirm the presence of a gestational sac in the uterus.
How to Handle an Early Intrauterine Pregnancy?
If a doctor determines that the estimated conception date doesn’t match the scan’s findings, a follow-up scan may be recommended. This allows for additional time for the embryo or pregnancy sac to develop, potentially confirming the conception date and ensuring the pregnancy is progressing at the expected rate.
What Causes an Early Intrauterine Pregnancy Failure?
Various factors can contribute to early intrauterine pregnancy failure or miscarriage. These include:
a. Chromosomal Abnormalities
Approximately 50% of miscarriages result from missing or extra chromosomes, which occurs randomly and is not inherited. This can lead to intrauterine fetal demise or blighted ovum.
b. Maternal Health Conditions
Preexisting maternal health conditions, such as uncontrolled diabetes, hormonal imbalances, serious infections, thyroid disease, or cervical and uterine issues, can increase the risk of miscarriage.
c. Age
Women over the age of 35 have a higher risk of miscarriage, which increases with age. Prior miscarriages also elevate the risk, but they do not necessarily prevent future successful pregnancies.
d. Lifestyle Factors
Lifestyle choices, such as smoking, heavy alcohol consumption, drug use, and extremes in weight, can significantly impact the likelihood of miscarriage.
Lowering Your Chances for Early Intrauterine Pregnancy Failure!
If you’ve been diagnosed with an early intrauterine pregnancy, consider these lifestyle adjustments to promote a healthy pregnancy:
– Retain a well-balanced diet with adequately of fruits and vegetables.
– Avoid alcohol, smoking, and abnormal use of drug.
– Maintain a healthy weight before conception.
– Address any identified health conditions before getting pregnant.
When to See a Doctor for Intrauterine Pregnancy?
As soon as you receive a positive pregnancy test result, it’s advisable to consult your healthcare provider. Vaginal bleeding or spotting, common signs of early intrauterine pregnancy period issues, should prompt immediate medical attention.
Should I Worry About IUP?
Intrauterine pregnancy, in itself, is not a cause for worry. In fact, it’s the desired and normal location for a pregnancy to develop. An IUP means that the fertilized egg has successfully implanted and is growing within the uterus, which is where a healthy pregnancy should be located. So, if you have confirmed that your pregnancy is intrauterine, there’s generally no need to worry about its location.
Is IUP a Symptom?
Intrauterine pregnancy is not a symptom itself. Instead, it is a medical term used to describe the location of a pregnancy within the uterus. Symptoms of pregnancy can include missed periods, breast tenderness, morning sickness, fatigue, and more. If you suspect you might be pregnant or are experiencing pregnancy-related symptoms, it’s advisable to take a pregnancy test and consult with a healthcare professional for confirmation and guidance.
What Is High-Risk Intrauterine Pregnancy?
A high-risk intrauterine pregnancy refers to a pregnancy that has an increased likelihood of complications or adverse outcomes. Several factors can contribute to a pregnancy being considered high-risk, including:
– Maternal age (very young or older than 35)
– Pre-existing medical conditions (i. e. diabetes, hypertension, or thyroid disorders)
– Multiple pregnancies (e.g., twins or triplets)
– A history of previous pregnancy complications
– Certain lifestyle factors (smoking, drug use, excessive alcohol consumption)
– Genetic factors or chromosomal abnormalities in the fetus
– Infections or conditions affecting the uterus
– According to doctors, 50 to 60% of intrauterine pregnancies survive with proper care and monitoring.
High-risk pregnancies require closer monitoring and specialized care to minimize risks and ensure the best possible outcome for both the mother and the baby. If you believe you may have a high-risk pregnancy or have been informed by your healthcare provider, it’s crucial to follow their recommendations and attend regular prenatal visits to manage any potential complications effectively.
Takeaway
Finally, understanding intrauterine pregnancy (IUP) is essential for expectant mothers and it’s a complex condition that can only be definitively diagnosed through ultrasound. If you suspect you have an early IUP, consult your doctor promptly. Remember that various maternal health conditions and genetic factors can influence the likelihood of IUP failure furthermore by taking proactive steps and seeking medical advice, you can enhance your chances of a healthy and successful pregnancy period.
FAQs
1. Can an ectopic pregnancy turn into an IUP naturally?
No, an ectopic pregnancy cannot naturally turn into an IUP. Ectopic pregnancies occur outside the uterus and are not viable.
2. Is an early intrauterine pregnancy more risky than a later one?
Not necessarily. The risk associated with an early IUP depends on various factors, including maternal health and genetic factors.
3. Can I prevent an early IUP failure?
While not all causes can be prevented, maintaining a healthy lifestyle, addressing health conditions, and seeking prompt medical care can lower the risk of early IUP failure.
4. Are all early IUP failures due to genetic issues?
No, early IUP failures can result from various factors, including maternal health conditions and lifestyle choices.
5. How soon should I see a doctor after a positive pregnancy test?
It’s advisable to see a doctor as soon as possible after a positive pregnancy test to monitor the progress of your pregnancy.